Bones! Bone health often goes unnoticed until something goes wrong. Unlike a twisted ankle or strained muscle, weakening bones don’t announce themselves with immediate painthey work silently, gradually becoming more fragile until a minor fall results in a serious fracture.
Understanding the warning signs of weak bones can be life-changing, literally. Early recognition allows for intervention that can strengthen bones, prevent fractures, and maintain the active lifestyle you value. More importantly, addressing bone health concerns now can prevent the devastating consequences of osteoporotic fractures later.
Understanding Bone Health: The Foundation of Mobility
Your bones are living tissues that constantly remodel themselves throughout your life. During childhood and young adulthood, your body builds bone faster than it breaks it down, resulting in increased bone mass. Peak bone mass typically occurs around age 30, after which the balance gradually shifts.
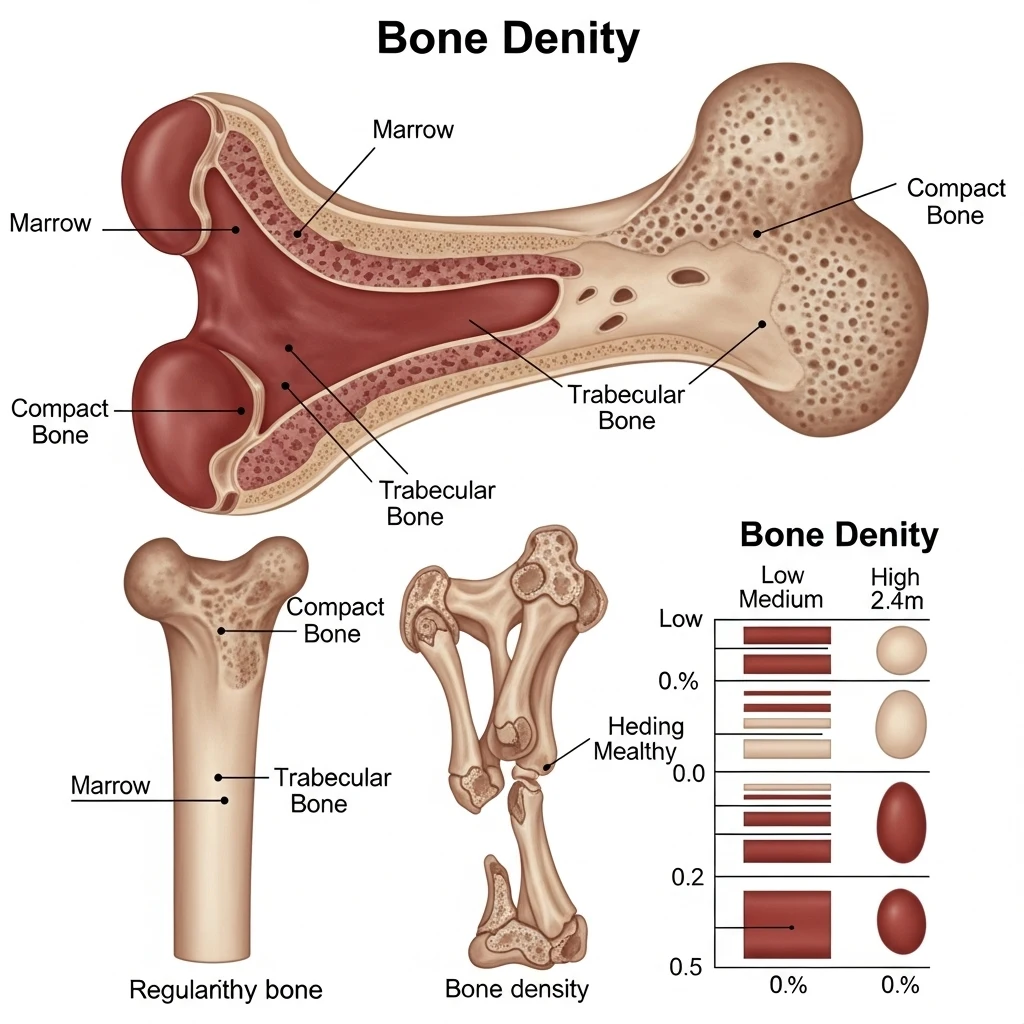
As we age, bone breakdown begins to outpace bone formation, leading to gradual bone density loss. While some bone loss is normal, excessive loss can result in osteoporosis – a condition where bones become so weak that minor stresses can cause fractures.
The Silent Nature of Bone Loss
Osteoporosis is often called the “silent disease” because bone loss occurs without symptoms. Many people don’t realize their bones have become dangerously weak until they experience their first fracture. By that point, significant bone density has already been lost, making treatment more challenging.
Warning Sign #1: Frequent or Easily Occurring Fractures
The most obvious sign of weak bones is fractures that occur with minimal trauma what doctors call “fragility fractures.”
What Constitutes a Fragility Fracture:
- Breaking a bone from a fall while standing or walking
- Fractures from activities that shouldn’t normally cause breaks
- Multiple fractures over a relatively short period
- Fractures in bones typically affected by osteoporosis (spine, hip, wrist, ribs)
Common Scenarios:
- Wrist fracture from catching yourself during a fall
- Rib fracture from coughing or sneezing forcefully
- Vertebral compression fracture from lifting or bending
- Hip fracture from a minor stumble
The Cascade Effect:
Having one osteoporotic fracture significantly increases your risk of additional fractures. Research shows that people who have had one vertebral fracture have a 5-fold increased risk of another vertebral fracture and a 2-fold increased risk of hip fracture.
Manisha, a 67-year-old retired teacher, didn’t think much of her wrist fracture from slipping in bathroom. “I figured it was just bad luck,” she recalls. When she fractured two ribs from a minor coughing fit six months later, her doctor ordered a bone density test that revealed severe osteoporosis. “I wish I’d known the wrist fracture was a warning sign.”
Warning Sign #2: Persistent Back Pain
Chronic back pain, particularly in the middle or lower back, can indicate vertebral compression fractures often the first sign of osteoporosis.
Characteristics of Osteoporosis-Related Back Pain:
- Gradual onset of pain without specific injury
- Pain that worsens with standing and improves when lying down
- Aching or sharp pain in the mid-back or lower back
- Pain that may radiate around the rib cage
- Discomfort that persists for weeks or months
Vertebral Compression Fractures:
These fractures occur when weakened vertebrae can no longer support the body’s weight and essentially collapse. Many happen without the person realizing they’ve had a fracture, attributed instead to “aging” or “arthritis.”
Silent Nature: Up to two-thirds of vertebral compression fractures cause no immediate symptoms, making them particularly insidious.
Progressive Impact: Multiple compression fractures can lead to significant height loss and spinal deformity over time.
Connection to Other Joint Problems:
Back pain from vertebral fractures can alter posture and gait, potentially contributing to problems in other joints. As discussed in our guide on weight loss for joint health, changes in spinal alignment can affect the entire kinetic chain, potentially impacting knee and hip function.
Warning Sign #3: Loss of Height or Developing a Stooped Posture
Gradual height loss and changes in posture often indicate multiple vertebral compression fractures.
Height Loss Red Flags:
- Significant height loss: More than 1.5 inches (4 cm) from your peak adult height
- Recent height loss: Any measurable height loss over 1-2 years
- Clothes fitting differently: Pants becoming too long, sleeves extending past your hands
- Difficulty reaching previously accessible shelves or cabinets
Postural Changes:
Kyphosis (Dowager’s Hump):
- Forward curvature of the upper spine
- Rounded shoulders and forward head posture
- Protruding abdomen despite no weight gain
- Difficulty standing fully upright
Functional Consequences:
- Reduced lung capacity due to compressed chest cavity
- Digestive issues from abdominal compression
- Balance problems and increased fall risk
- Social and psychological impact from changed appearance
Early Detection Importance:
Regular height measurements at doctor visits can detect bone loss before severe deformity develops. Simple wall measurements at home can also track changes over time.
Warning Sign #4: Limited Mobility and Increased Fall Risk
Weak bones often coincide with muscle weakness and balance problems, creating a dangerous combination.
Mobility Changes Suggesting Bone Weakness:
- Increased difficulty getting up from chairs
- Trouble climbing stairs or walking on uneven surfaces
- Reduced confidence in movement and balance
- Fear of falling that limits activity
- Decreased grip strength and overall muscle power
The Bone-Muscle Connection:
Bones and muscles work together in complex ways:
- Mechanical loading: Muscle contractions stimulate bone formation
- Shared risk factors: Aging, inactivity, and hormonal changes affect both
- Nutritional factors: Vitamin D and protein deficiency impact both bone and muscle health
- Activity dependence: Both require regular use to maintain strength
Balance and Fall Risk:
- Poor bone health often accompanies balance problems
- Fear of falling can lead to further activity reduction
- Reduced activity creates a cycle of worsening bone and muscle weakness
- Environmental hazards become more dangerous with fragile bones
This connection becomes particularly important for patients considering joint procedures. As explored in our articles on knee replacement alternatives and hip replacement options, bone health significantly impacts surgical outcomes and recovery.
Warning Sign #5: Additional Risk Factors and Subtle Signs
Several other indicators may suggest weakening bones:
Dental Health Changes:
- Tooth loss or loose teeth: May indicate jawbone deterioration
- Receding gums: Can reflect overall bone loss
- Ill-fitting dentures: May suggest continued jawbone loss
Nail and Hair Changes:
- Brittle or easily broken fingernails
- Hair thinning or loss
- Changes in nail growth patterns
These signs often reflect nutritional deficiencies or hormonal changes that also affect bone health.
Grip Strength Reduction:
- Difficulty opening jars or bottles
- Weakened handshake
- Problems with fine motor tasks
Grip strength correlates with overall bone density and fracture risk, making it a useful screening tool.
Who’s at Risk: Understanding Your Vulnerability
Primary Risk Factors:
Age and Gender:
- Women over 50, especially post-menopause
- Men over 70
- Early menopause (before age 45)
Medical Conditions:
- Rheumatoid arthritis and other inflammatory conditions
- Celiac disease and other malabsorption disorders
- Chronic kidney disease
- Hyperthyroidism
- Eating disorders
Medications:
- Long-term corticosteroid use
- Some anti-seizure medications
- Certain cancer treatments
- Proton pump inhibitors (long-term use)
Lifestyle Factors:
- Smoking and excessive alcohol consumption
- Sedentary lifestyle
- Low calcium and vitamin D intake
- Excessive caffeine consumption
Family History Importance:
Having a parent who suffered a hip fracture doubles your risk of hip fracture, regardless of your bone density measurements.
The Diagnostic Process: Confirming Bone Health
Bone Density Testing (DEXA Scan):
- Gold standard: Dual-energy X-ray absorptiometry (DEXA)
- Painless procedure: Takes 10-30 minutes
- T-score interpretation:
- Normal: -1.0 and above
- Osteopenia (low bone mass): -1.0 to -2.5
- Osteoporosis: -2.5 and below
Additional Testing:
Laboratory Tests:
- Vitamin D levels
- Calcium metabolism markers
- Thyroid function
- Bone turnover markers
Imaging Studies:
- Spine X-rays to detect existing fractures
- CT scans for detailed bone structure assessment
- MRI for acute fracture evaluation
Prevention and Treatment Strategies
Lifestyle Modifications:
Exercise Programs:
- Weight-bearing exercises: Walking, dancing, hiking
- Resistance training: Helps build both bone and muscle strength
- Balance training: Reduces fall risk
- Flexibility work: Maintains mobility and posture
Nutrition Optimization:
- Adequate calcium: 1,000-1,200 mg daily for most adults
- Sufficient vitamin D: 800-1,000 IU daily
- Protein adequacy: Essential for bone matrix formation
- Limited alcohol and caffeine
Medical Interventions:
Medications When Appropriate:
- Bisphosphonates for established osteoporosis
- Hormone replacement therapy in specific situations
- Newer treatments like denosumab or teriparatide for severe cases
- Calcium and vitamin D supplementation
Fall Prevention:
- Home safety modifications
- Vision and hearing optimization
- Medication review to minimize fall risk
- Balance training programs
The Impact on Surgical Outcomes
Poor bone health significantly affects orthopedic surgery outcomes:
Joint Replacement Considerations:
- Implant fixation: Weak bones may not hold implants securely
- Healing time: Osteoporotic bone heals more slowly
- Fracture risk: Higher risk of periprosthetic fractures
- Revision surgery: May be more complex with poor bone stock
For patients considering procedures detailed in our guides on robotic vs. traditional knee replacement or hip replacement recovery, addressing bone health beforehand can significantly improve outcomes.
Pre-surgical Optimization:
- Bone density assessment and treatment
- Nutritional optimization
- Exercise programs to strengthen bones and muscles
- Fall prevention strategies
When to Seek Professional Evaluation
Immediate Consultation Needed:
- Any fracture from minor trauma
- Sudden onset of severe back pain
- Noticeable height loss over short periods
- Multiple risk factors combined with symptoms
Preventive Evaluation Recommended:
For Women:
- Age 65 and older (routine screening)
- Post-menopause with risk factors
- Estrogen deficiency at any age
For Men:
- Age 70 and older (routine screening)
- Age 50-69 with risk factors
- Low testosterone levels
Regular Monitoring:
- Follow-up DEXA scans every 2 years for osteoporosis
- Annual evaluations for those on bone medications
- Reassessment after fractures or significant medical changes
Living Well with Weak Bones
Having weak bones doesn’t mean accepting a sedentary, fearful lifestyle:
Staying Active Safely:
- Choose appropriate exercises with proper supervision
- Modify activities to reduce fall risk while maintaining fitness
- Use assistive devices when needed without shame
- Focus on what you can do rather than limitations
Home Environment Optimization:
- Remove tripping hazards like loose rugs
- Ensure adequate lighting throughout the home
- Install grab bars in bathrooms and stairways
- Use non-slip surfaces in wet areas
Building Confidence:
- Education about your condition and treatment options
- Participation in support groups or programs
- Working with healthcare providers who understand your goals
- Celebrating improvements and maintaining hope
The Connection to Overall Health
Bone health reflects and influences overall health:
Cardiovascular Health:
- Some bone medications affect cardiovascular risk
- Exercise beneficial for both bones and heart
- Shared nutritional requirements
Mental Health:
- Fractures can lead to depression and anxiety
- Fear of falling can create social isolation
- Maintaining independence crucial for emotional well-being
Nutritional Status:
- Bone health reflects overall nutritional adequacy
- Digestive health affects nutrient absorption
- Medication interactions may impact nutrition
The Bottom Line: Early Recognition Saves Lives
Recognizing the warning signs of weak bones can literally be life-saving. Hip fractures, in particular, carry significant mortality risk up to 20% of people who suffer hip fractures die within one year, often from complications related to immobility.
Key takeaways for bone health awareness:
- Don’t dismiss “minor” fractures they may indicate significant bone weakness
- Persistent back pain deserves evaluation, especially in those at risk
- Height loss and posture changes often indicate multiple vertebral fractures
- Mobility problems may reflect both bone and muscle weakness
- Early intervention can prevent fractures and maintain independence
The Prevention Advantage:
Unlike many aspects of aging, bone loss is largely preventable and often treatable. The earlier you recognize warning signs and take action, the better your outcomes.
Working with Healthcare Providers:
Choose providers who:
- Take bone health seriously across all age groups
- Understand the connection between bone health and overall mobility
- Offer comprehensive evaluation and treatment options
- Support your goals for maintaining an active lifestyle
Your bones are the foundation of your mobility and independence. Paying attention to warning signs, seeking appropriate evaluation, and taking preventive action can help ensure that your skeletal system continues to support your active lifestyle for decades to come.
Whether you’re noticing early warning signs or simply want to optimize your bone health proactively, professional evaluation and guidance can help you develop a comprehensive plan for maintaining strong, healthy bones throughout your life.
Don’t wait for a fracture to discover that your bones need attention. The warning signs are there learning to recognize and act on them can make the difference between a fracture-free future and a life limited by fragile bones.


Leave a Reply